What is oral cancer?
Oral cancer starts in the cells of the mouth. A cancerous (malignant) tumour is a group of cancer cells that can grow into and destroy nearby tissue. It can also spread (metastasize) to other parts of the body. The most common place oral cancer spreads to is the lymph nodes in the neck. Oral cancer may also be called oral cavity cancer or mouth cancer.
Cells in the mouth sometimes change and no longer grow or behave normally. These changes may lead to non-cancerous (benign) tumours such as warts and fibromas.
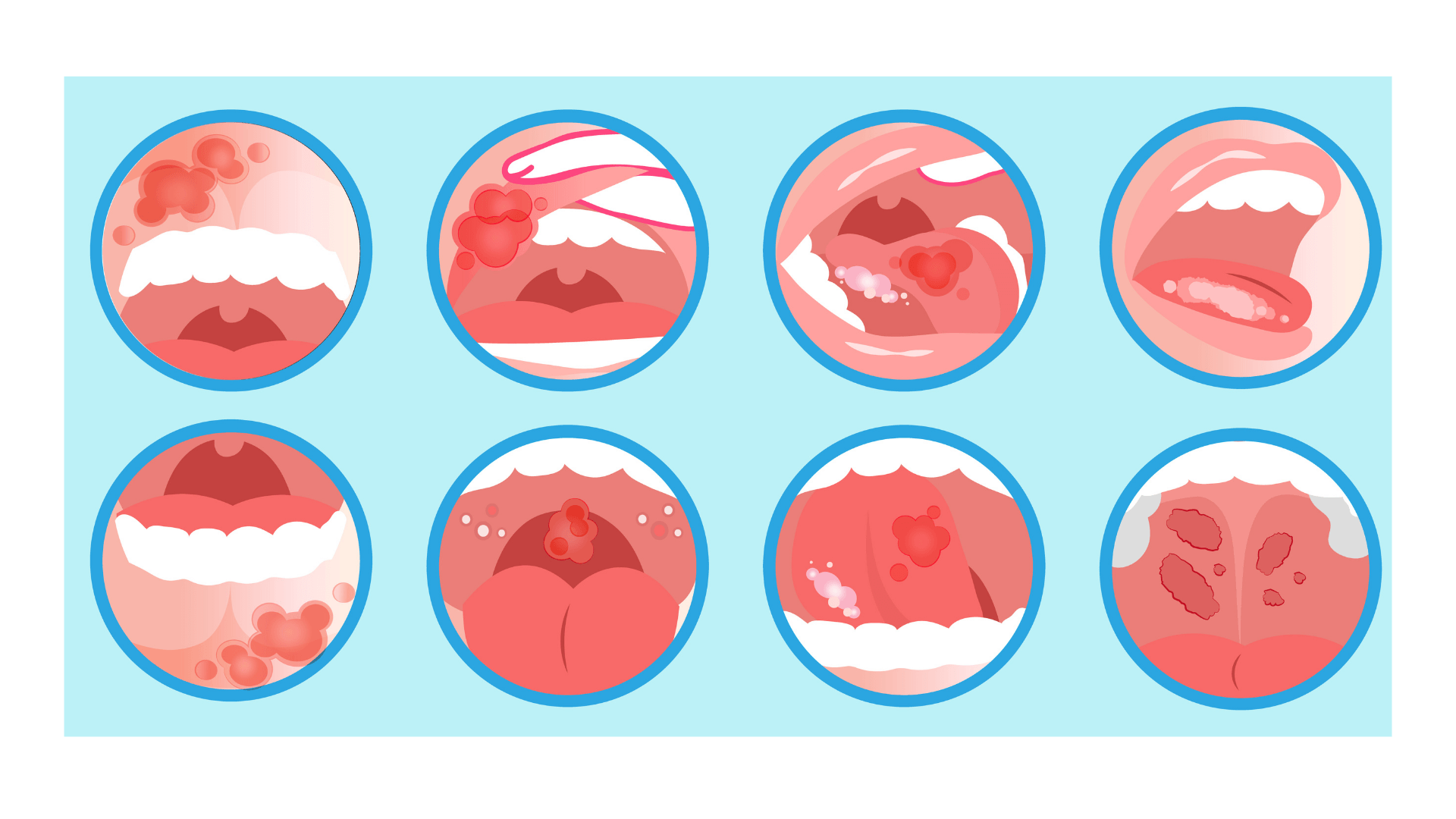
Changes to cells of the mouth can also cause pre-cancerous conditions. This means that the abnormal cells are not yet cancer, but there is a chance that they may become cancer if they aren’t treated. The most common pre-cancerous conditions of the mouth are leukoplakia and erythroplakia.
But in some cases, changes to the cells of the mouth can cause oral cancer. The mouth is covered by a lining called the oral mucosa (mucous membrane). The oral mucosa is made up of squamous cells called the squamous epithelium. Most often, oral cancer starts in these flat, thin squamous cells. This type of cancer is called squamous cell carcinoma of the mouth.
Rare types of oral cancer can also develop. These include salivary gland cancer and melanoma.
Cancerous tumours of the mouth
A cancerous tumour of the mouth can grow into and destroy nearby tissue. It can also spread (metastasize) to other parts of the body. Cancerous tumours are also called malignant tumours.
Squamous cell carcinoma
- The most common type of oral cancer is squamous cell carcinoma (SCC). SCC starts in the flat, thin cells (called squamous cells) that make up the oral mucosa (mucous membrane).
Rare mouth tumours
- salivary gland cancer
- melanoma
- bone and soft tissue sarcoma
- Lymphoma
Pre-cancerous conditions
Pre-cancerous conditions of the mouth are changes to cells of the mouth that make them more likely to develop into cancer. These conditions are not yet cancer. But if they aren’t treated, there is a chance that these abnormal changes may become oral cancer.
The most common pre-cancerous conditions of the mouth are leukoplakia and erythroplakia.
Leukoplakia
Leukoplakia is an abnormal white or grey area that develops on the tongue, the inside of the cheek, the gums or the floor of your mouth.
The presence of leukoplakia does not necessarily mean cancer. The risk of developing oral cancer depends on how different the abnormal cells are in shape, size and appearance compared to normal mouth cells. This abnormality is called dysplasia. The healthcare team closely watches people who have leukoplakia to look for signs of cancer.
Risk factors
The following risk factors increase your chance of developing leukoplakia:
- smoking heavily
- chewing tobacco
- excessive alcohol use

Signs and symptoms
The signs and symptoms of leukoplakia include a whitish area or spots inside the mouth that cannot be easily scraped off.
Diagnosis
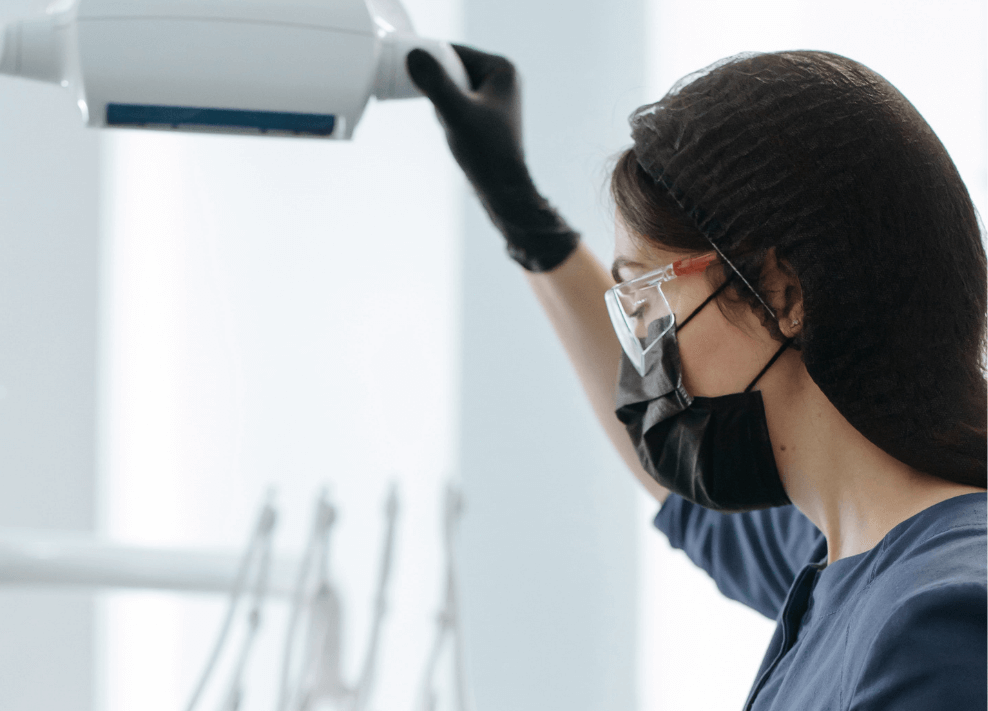
Your dentist or doctor will ask you about any symptoms you have and do a dental or oral exam. They may take a sample of cells from the abnormal area (called a biopsy) so they can be tested in a lab.
Treatments
There are no standard treatments for leukoplakia. It is managed by active surveillance. This means that your healthcare team watches your condition closely. They will use regular tests and exams to find any cancerous change early.
Because leukoplakia can develop into cancer, people with this condition should avoid known risk factors, such as using tobacco and drinking alcohol.

Erythroplakia
Erythroplakia is an abnormal red area or group of red spots that forms on the mucous membrane lining the mouth, with no clear cause. The presence of erythroplakia does not necessarily mean cancer, but this pre-cancerous condition has a high risk of developing into cancer. About 50% of these lesions develop into squamous cell carcinoma.
Risk factors for erythroplakia
Smoking heavily
chewing tobacco
excessive alcohol use
Signs and symptoms
The signs and symptoms of erythroplakia include a raised or smooth red area that often bleeds when scraped.
Diagnosis
Your dentist or doctor will ask you about any symptoms you have and do a dental or oral exam. They may take a sample of cells from the abnormal area (called a biopsy) so they can be tested in a lab.
Treatments
Treatment options for erythroplakia may include:
- careful watching (active surveillance) and frequent follow-up
- surgery
- cryosurgery
- laser surgery
Because erythroplakia can develop into cancer, people with this condition should avoid known risk factors, such as using tobacco and drinking alcohol.
Risk factors for oral cancer
A risk factor is something that increases the risk of developing cancer. It could be a behaviour, substance or condition. Most cancers are the result of many risk factors. Tobacco and alcohol are the most important risk factors for oral cancer.
Oral cancer is rare in children and young adults. The risk of developing oral cancer increases with age and is greatest after 45 years of age. More men than women develop oral cancer, and it occurs more often in men of African descent.
Pre-cancerous conditions of the mouth include leukoplakia and erythroplakia. They aren’t cancer, but they can sometimes become oral cancer if they aren’t treated. Some of the risk factors for oral cancer may also cause these pre-cancerous conditions.
Risk factors are generally listed in order from most to least important. But in most cases, it is impossible to rank them with absolute certainty.
Known risk factors
There is convincing evidence that the following factors increase your risk for oral cancer.
Tobacco
Most oral cancers are linked to tobacco use. All forms of tobacco increase the risk for this cancer, including cigarettes, cigars, pipes, bidis and smokeless tobacco (including chewing tobacco and snuff). The longer you use tobacco and the more you use, the greater your risk. The risk for oral cancer greatly increases when smoking is combined with using smokeless tobacco, drinking alcohol or both. Continuing to smoke after treatment for oral cancer increases the risk of developing a second oral cancer.
Smoking cigarettes, cigars or pipes increases the risk for oral cancer. These products are often linked with cancer of the lip if they sit on the lips. Using smokeless tobacco products is linked with cancer of the gums and inner lining of the cheeks and lips because the tobacco regularly touches these areas.
Some studies show that second-hand smoke may also increase the risk for oral cancer.
Alcohol
Alcohol is one of the main risk factors for oral cancer. The more you drink, the greater your risk. Using alcohol and tobacco together increases the risk of developing oral cancer more than using either one alone.

Betel quid and areca nut
Chewing betel quid or areca nut is common in South Asia and among some South-Asian immigrants in Canada. Betel quid, or paan, is areca nut (the seed from the fruit of the oriental palm) and lime wrapped in a betel leaf. Some people chew areca nut by itself. Betel quid and tobacco are often chewed together, or betel quid may contain tobacco.
Betel quid and areca nut contain cancer-causing substances. People who chew betel quid or areca nut have a higher risk of developing oral cancer, especially in the inner lining of the cheeks and lips.
Human papillomavirus (HPV)
HPV is a group of more than 100 different types of related viruses. Many types of HPV are spread through sexual contact, including oral sex. They can infect the sexual organs (the penis in men or the vulva, vagina and cervix in women), the rectum and the anus. They can also infect the mouth and throat.
The different types of HPV are usually given a number to identify them. Infection with HPV-16 increases the risk of oral cancer. Infection with HPV-18 may also increase the risk. HPV is likely the cause of oral cancer that is not linked with tobacco or alcohol use.
Previous cancer
People who have had oral cancer have a higher risk of developing another oral cancer, especially if they continue to use tobacco or alcohol. Having cancer of the esophagus, larynx, lung or cervix also increases your risk of oral cancer.

Family history of squamous cell carcinoma (SCC)
SCC is the most common type of oral cancer. There is a higher risk of developing SCC in the head and neck region (including the mouth) if a first-degree family member (parent, sibling or child) has been diagnosed with SCC of the head and neck.
Sun exposure
Sun exposure increases the risk of developing lip cancer. This is especially true for people who work in the sun for long periods of time, such as farmers. Fair-skinned people also have a greater risk of developing lip cancer. Most lip cancers occur on the bottom lip, likely because it’s more exposed to the sun.
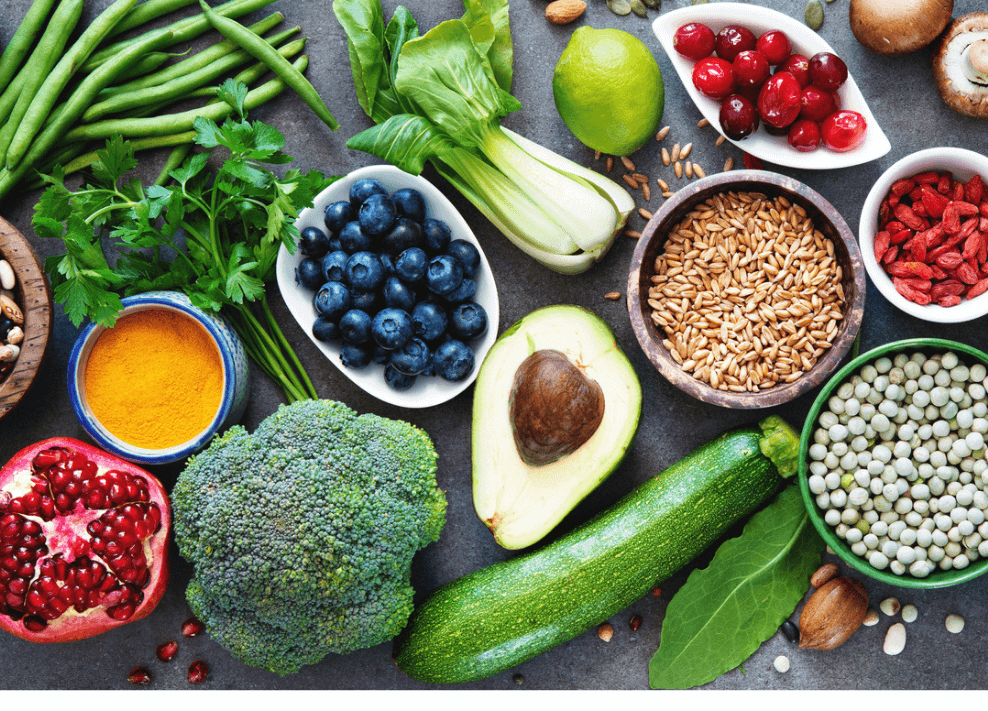
Diet low in vegetables and fruit
Many studies show that not eating enough vegetables and fruit increases the risk of developing oral cancer. Substances like carotenoids, which are common in vegetables and fruit, are linked with a lower risk of oral cancer.
Weakened immune system
Your immune system can be weakened after an organ transplant or treatment for an immune system disease. People with a weakened immune system have a higher risk of developing oral cancer, especially lip cancer. The higher risk may be due to taking drugs that suppress your immune system. People with weakened immune systems are also more likely to get an HPV infection, which increases the risk for oral cancer.
Graft-versus-host disease (GVHD)
People who have a stem cell transplant may develop GVHD. GVHD is when the healthy transplanted stem cells see the body as foreign and start to destroy the body’s cells, including cells in the mouth. Damage to cells in the mouth from GVHD increases the risk of developing oral cancer.
Lichen planus
Lichen planus is a chronic condition that forms a rash or sores on the skin and inside the mouth, usually on the tongue, gums and lining of the cheeks. Sometimes the sores can develop into ulcers. Having lichen planus with ulcers in the mouth for a long time increases the risk of developing oral cancer.
Poor oral health
People with poor oral health may have several missing teeth, bleeding gums or chronic infections from bacteria and viruses like HPV. They may not go to the dentist very often to take care of their mouth. Studies show that people with poor oral health have a higher risk of developing oral cancer.
Inherited conditions
An inherited, or genetic, condition is passed from parents to their children through genes. People with the following inherited conditions have a higher risk of developing pre-cancerous changes in the mouth and oral cancer. These develop at a much earlier age than oral cancer caused by other risk factors.
Fanconi anemia is a rare genetic condition that affects the bone marrow so it can’t make enough red blood cells, white blood cells or platelets.
Dyskeratosis congenital is a genetic syndrome that can cause abnormal red blood cells, skin rashes and abnormal fingernails and toenails.

Possible risk factors
The following factors have been linked with oral cancer, but there is not enough evidence to show they are known risk factors. More research is needed to clarify the role of these factors for oral cancer.
Poor-fitting dentures
A few studies found that having dentures that don’t fit properly can increase the risk for oral cancer. This may because the dentures rub on the gums and cause sores that may develop into a cancerous tumour.
Drinking very hot beverages
Some studies found that people who drink very hot beverages may have a higher risk for oral cancer. The hot beverage may cause damage to the cells in the mouth, which may develop into a cancer.
Reducing your risk for oral cancer
Don’t smoke at all and avoid smokeless tobacco The best way to reduce your risk for oral cancer is to avoid all forms of tobacco, including cigarettes, cigars, pipes, chewing tobacco, snuff, and second-hand smoke.
If you do smoke, get help to quit. Quitting reduces your risk for oral cancer. Former smokers have a lower risk of oral cancer than current smokers. The longer you go without smoking or suing smokeless tobacco, the lower your risk of developing oral cancer.
Limit the amount of alcohol you drink
The less alcohol you drink, the lower your risk of developing oral cancer. If you choose to drink alcohol, keep it to less than 1 drink per day if you’re a woman and less than 2 drinks per day if you’re a man.
Don’t smoke or use smokeless tobacco if you drink alcohol. Using tobacco and alcohol together increases the risk for oral cancer more than using either one alone.
Avoid chewing betel quid or areca nut
Chewing betel quid or areca nut increases your risk of developing oral cancer. Betel quid, or paan, is areca nut (the seed from the fruit of the oriental palm) and lime wrapped in a betel leaf. Some people chew areca nut by itself.
Chewing betel quid or areca nut is common in South Asia and among some South-Asian immigrants in Canada.
Get vaccinated against human papillomavirus (HPV)
HPV can infect the mouth, especially if you have oral sex and multiple sexual partners. The 3 HPV vaccines available in Canada are Gardasil, Cervarix and Gardasil 9. These vaccines help protect against infection with HPV-16 and HPV-18, the 2 types of HPV linked with different types of cancer, including oral cancer. Gardasil 9 also protects against 5 other types of HPV that can cause cancer.
These vaccines help lower the risk of HPV-related cancers, like cervical cancer. Recent studies show that they may also help lower the risk of oral and throat cancers, but more research is needed.
Get vaccinated or have your children vaccinated through school-based programs where available. If you are not eligible for a free vaccination, talk to your doctor about which vaccine is right for you and when you should have it.

Reduce your exposure to HPV
The only sure way to prevent HPV infection is to completely avoid any genital contact with another person. If you are young, delay having sex. If you are sexually active, you can reduce your risk of exposure to HPV by:
• having as few sexual partners as possible
• being in a monogamous relationship with someone who hasn’t had a lot of sexual partners
• using a condom
Using a condom can lower the risk of HPV infection if it is put on before skin-to-skin sexual contact. However, areas not covered by a condom still allow some skin-to-skin contact during sexual activity. So using condoms will reduce, but not eliminate, the risk of HPV infection.
Protect yourself from the sun
When you are outside, use a lip balm with SPF to help lower your risk for lip cancer. Seek shade or create your own shade. Wear a hat with a wide brim that covers your head, face, ears and neck.
Reduce the amount of time you spend in the sun between 11 a.m. and 3 p.m., when the sun’s rays are at their strongest, or any time of the day when the UV Index is 3 or more. In Canada the UV Index can be 3 or more from 11 a.m. to 3 p.m. between April and September, even when it’s cloudy.
Eat vegetables and fruit
Eating a variety of vegetables and fruit each day protects against oral cancer. Carotenoids are substances found in yellow and orange vegetables and fruit as well as dark green vegetables. Studies show that carotenoids lower the risk of oral cancer by limiting damage to cells in the mouth.
Practise good mouth care
Good mouth care means keeping all of your mouth, including your teeth, gums and tongue, clean and healthy. Brush your teeth after meals and before you go to bed. Floss your teeth every day. If you wear dentures, clean them every day. When your dentures don’t fit properly or cause sore spots in your mouth, talk to your dentist about having them fitted again.
Have regular checkups by your dentist, even if you don’t have natural teeth. Your dentist can help find and treat problems in the mouth that could lead to cancer.
Find out if you’re at high risk
Some people have a higher-than-average risk for oral cancer. This includes people who have already had oral cancer, who are at a higher risk of developing another oral cancer. Talk to your doctor about your risk. If it’s higher than average, you may need to visit your doctor or dentist more often to check the mouth for cancer.

